- Be able to describe the organization and function of thymus, lymph nodes, spleen and tonsils.
- Be able to identify the regions rich in B and T lymphocytes in each organ and explain the cellular processes, relevant to immune functions, that are taking place in these regions.
- Know the homing patterns of B & T lymphocytes.
There is a continuous production and recirculation of lymphocytes in the body. Many of the lymphocytes you see in blood vessels, lymphatic vessels or in tissue have been exposed to antigen and are thus poised to respond to specific antigenic stimuli. The lymph nodes and the spleen facilitate immunological surveillance of the host. They are the sites of 1) antigen trapping, 2) homing of cells of the immune system that have been exposed to their triggering antigens, and 3) subsequent expansion and release of lymphocyte clones capable of further response to specific antigens. The exposure of lymphocytes to antigens occurs in solitary lymph nodes (follicles), in aggregates of lymph nodes present beneath mucous membranes, and in the spleen. The palatine tonsils and the Peyer’s patches in the ileum (not seen in this laboratory) consist of multiple aggregates of lymph nodes. T lymphocytes, which participate in cell-mediated immunity or modulate the immune responses of other cells, differentiate in the thymus during childhood. B lymphocytes, which have the capacity to become plasma cells and secrete immunoglobulins, differentiate in the bone marrow throughout life.
Slide 027 Lymph node H&E View Virtual Slide
Slide 026 20X Lymph nodes H&E View Virtual Slide
Slide 026 40X Lymph node H&E View Virtual Slide
Slide 142 Lymph node H&E View Virtual Slide
Slide 030 Mesentery H&E View Virtual Slide
Slide 028 Lymph node silver View Virtual Slide
Use slide 27 to study the overall organization of a lymph node and identify the cortex, medulla and hilus (Slide 027 View Virtual Slide). Some slides do not show a medulla or hilus, depending on the plane of section, especially, the hilus. The hilar region is rather small and will not be present in all slides. Using slide 27 and other slides, locate the capsule, lymphatic follicles or nodules (B cell-rich), the diffuse or deep cortical zone (T cell-rich), in addition to the medulla and the hilus. Recall that the deep cortex is the zone of antigen presentation, while T cell help occurs in the follicles. What is the distribution of B cells and T cells in the lymphatic tissue?
Answer
The thymus is entirely composed of T cells, epithelial reticular cells and some macrophages. Occasionally another type of cell will get into the thymus, but it does not belong there. The thymus consists of a cortex and medulla with no germinal centers. Immature T cells are found at the edges of the cortex. As they mature, they migrate deeper into the cortex and eventually leave as mature naïve T cells through the venules of the medulla. In the lymph node, the cortex is made of primary follicles of resting B cells and secondary follicles with germinal centers. The germinal centers are where B cells are undergoing clonal expansion, after binding antigen and receiving T cell help. Most T cells are located deeper in the cortex. Antigen-stimulated helper T cells are formed when antigen is presented to them by dendritic cells (and possibly macrophages), deep in the cortex. B cells also bind their antigen in this region. B cells entering the lymph node travel through the cortex to a follicle. If they have bound antigen in the cortex, they attract antigen-stimulated T helper cells to the follicle, where T cell help occurs. T cell help in the spleen occurs in the PALS. Close to, if not touching, the PALS are follicles of resting B cells, a clone of which may give rise to a germinal center upon proper stimulation.
Generally the sinuses show up best beneath the capsule (subcapsular sinus) in either slide 026 View Image [orientation] or slide 142 View Image [orientation] or in the medulla (medullary sinuses, see below). Make sure you have found a real sinus and not just a separation artifact. You should be able to see: 1) reticular cells spanning the sinus, 2) some endothelial cell nuclei defining the inner wall of the sinus (adjacent to the lymphatic follicles), and 3) circulating lymphocytes and macrophages in the lumen. What is a fiber associated reticular cell?
Answer
These are the stellate shaped fibroblasts found in the lymph node that are involved in making reticular (type III collagen) fibers. They are NOT the same as the epithelial reticular cells found in the thymus: epithelial reticular cells s are true epithelial cells derived from the endodermal lining of the third pharyngeal pouch in the embryo (the third pouch is what gives rise to the thymus) whereas reticular cells, like most connective tissue fibroblasts, are derived primarily from mesoderm.
Afferent lymphatic vessels that penetrate the capsule are difficult to identify, but can be observed in slide 030 View Image. If you see venule-sized vessels adjacent to or within the capsule you can make the provisional identification of an afferent lymphatic vessel, especially if these vessels contain lymphocytes and show valves. With the low power objective find primary and secondary follicles (follicles with germinal centers, best seen in slide 27 View Image) . It is not always possible to distinguish primary and secondary follicles because a glancing section through a secondary follicle may miss the germinal center and thus mimic a primary follicle, and that sometimes the boundary between the follicles and the diffuse lymphatic cortex is indistinct. The germinal centers slide 27 View Image [orientation] in these particular specimens are at an end stage; that is, blastogenesis has already occurred and most of the cells present in the center are simply reticular cells and a few macrophages. Recall that the germinal centers are the sites of T cell help, B lymphocyte proliferation and antigen-dependent differentiation of B cells into lymphoblasts. The lymphoblasts continue to differentiate into plasma cells and memory B cells. Where do the plasma cells in the lymph node go?
Answer
Nowhere. Once a plasma cell differentiates in the lymph node, it generally migrates to a medullary cord in the medulla of the lymph node and begins secreting antibodies that travel throughout the body (first through efferent lymphatics that then drain into venous blood). Once in the medullary cord, the plasma cell generally stays puts. It is worth noting that plasma cells are rarely observed in peripheral blood. The numerous plasma cells found in various tissues in the body traveled in the circulation as naive B lymphocytes until they were stimulated to enter the peripheral tissue and differentiate into a plasma cell locally.
Make sure that you find the high endothelial venules (specialized cortical veins lined by high endothelium) especially visible in either slide 27 View Image or slide 142 View Image. How do cells travel from the blood to the lymph node?
Answer
There are many adhesion molecules and receptors expressed both by the high endothelial post capillary venules of the lymph node and on the B and T lymphocytes that allow them to enter the lymph node. This process is called "lymphocyte homing". When appropriate signals are received, cells begin to cross the endothelial cells of the venules. Finally they reach the deep cortex where they can receive T cell help and continue on to the follicles.
With a low power objective locate the medullary cords and sinuses in either slide 026 View Image or slide 142 View Image. Find endothelial lining cells, reticular cells, circulating lymphocytes and macrophages (that may appear foamy after having engulfed some RBCs). Review the blood supply to the node. In slide 27 View Image, a number of efferent lymphatic vessels with valves can be found in the hilar connective tissue. Now look at slide 28 to review the role of reticular fibers in supporting the structure of the lymph node.
Slide 161 gastroduodenal junction H&E View Virtual Slide
Slide 157b fundic stomach H&E View Virtual Slide
Slide 175 Appendix H&E View Virtual Slide
Slide UCSF 261 appendix H&E View Virtual Slide (virtual slide courtesy of the University of California, San Francisco)
Slide 168 Small intestine, jejunum H&E View Virtual Slide
Solitary lymphatic nodules are present throughout the GI tract, respiratory tract and, to a lesser extent, the urinary tract. Look for solitary nodules in slide 161 (the gastro-duodenal junction). At low power, localize the duodenum by identifying mucous glands (Brunner’s glands) in the submucosa and, then, look for discrete basophilic nodules (follicles) slide 161 View Image in the lamina propria or in the submucosa in the midst of mucous glands, some of which will have germinal centers. Solitary lymphatic nodules can be also seen in our slides of the stomach (slide 157b fundic stomach H&E View Image) and the appendix (slide 175 View Image). Many such nodules combined give rise to named structures, such as tonsils or "Peyer’s patches." The term, Peyer’s patches, specifically refers to aggregates of lymphatic nodules in the ileum, but often the term is used mistakenly to describe any aggregates of lymphatic nodules in other parts of the GI tract. In addition to lymphoid aggregates and nodules present in the lamina propria and submucosa are intraepithelial lymphocytes, which are T-cells that develop in the thymus and migrate into various epithelial tissues in the skin, GI, respiratory, and genitourinary tracts where they serve an important function as a first line of defense against pathogens. You can find intraepithelial lymphocytes in most slides of these organ systems, but they are probably easiest to see in slide 168. Look for small, dark, round nuclei slide 168 View Image situated between the epithelial cells.
Slide 138 20X Tonsil palatine H&E View Virtual Slide
Slide 138 40X Tonsil palatine H&E View Virtual Slide
Slide 138L tonsil faucial H&E View Virtual Slide
Using slide slide 138L, observe the numerous aggregates of lymphatic follicles with germinal centers and the stratified squamous epithelium that covers the oral surface of these aggregates. The epithelium also lines crypts that dip into underlying lymphatic nodules. The epithelium lining some crypts is almost obliterated by infiltrating lymphocytes. Some crypts will probably be cut in cross section so continuity with the oral cavity will not be apparent. At 10X, locate a follicle with a germinal center. Note small, lightly stained areas (they almost look like small holes) distributed throughout the center. If you can’t find them look at another germinal center. These lightly stained areas are macrophages slide 138 View Image in the germinal center. Look at them with high power. You should see a large cell with a large, vesicular nucleus that contains at least one conspicuous nucleolus. You will have to work to see them, but once you’ve seen one you will be able to recognize them in most lymphatic tissue (e.g., slide 175 View Image). The cytoplasm of these macrophages will have a variable appearance but will usually include two or three hyperchromatic spheres that are ingested B lymphocytes that failed to differentiate properly and underwent apoptosis. In slide slide 138 20x, locate the dense, irregular connective tissue capsule slide 138 View Image that separates the tonsil from the rest of the pharynx tissue. However, the connective tissue capsule does not completely enclose any of the tonsils. There are also a few mucous glands and muscle fibers included in this section.
Slide 147B Spleen H&E View Virtual Slide
Slide 148 20X Spleen H&E View Virtual Slide
Slide 148 40X Spleen H&E View Virtual Slide
Slide 301 spleen H&E View Virtual Slide
Of the two human slides, slide 147 is better in that it is more compact and the content of erythrocytes is reduced. With low power try to distinguish between the red and white pulp. Think about why these terms are employed. While the white pulp has an obvious role in the immune response, don’t forget the role of the red pulp in potential antigen trapping by macrophages. Find the capsule slide 147B View Image and trabeculae slide 147B View Image (containing trabecular arteries and veins—you may find just one or the other). Much of the white pulp you will see in your section of slide 147 is composed of B-cell dependent follicles, showing germinal centers. Slide 148 contains little easily recognizable white pulp (somewhat abnormal) but is helpful in seeing the periarteriolar lymphatic sheath (PALS) slide 148 View Image that surround central arteries (which range in size from small arteries to arterioles). Recall that the PALS contains mostly T lymphocytes and is homologous with the deep cortical zone of a lymph node. Going back to slide 147, you'll see many instances where a PALS is expanded eccentrically to include a lymphatic follicle slide 147B View Image, usually with a germinal center; recall that these follicles are B-cell rich. With this expansion, the "central" artery is pushed off to one side and therefore not very "central." Many texts and atlases usually show this classic view of a the central artery and its PALS in cross section. However, you should realize that the PALS is a sheath that runs along the length of each central artery, and you can see this particularly well in slide 301 View Image. The marginal zone slide 148 View Image [orientation] is a region surrounding the white pulp that is difficult to recognize unless the spleen is very well preserved and sectioned, or, as in slide 148, the red pulp is particularly obvious (here the red pulp is packed with erythrocytes). This region contains mostly reticular cells and antigen-presenting cells, as well as some lymphocytes that may play a role in antigen trapping or processing. Don't get too hung up on trying to definitively demarcate the marginal zone in these sections, but you should have a general idea of this transition zone between white pulp and red pulp and understand its function as a primary site of antigen presentation in the spleen. In the red pulp, identify the splenic cords (tissue between the sinuses) and venous sinuses that are reasonably well preserved beneath the capsule in slide 147B View Image [orientation]. The cords and sinuses show up particularly well in slide 148 View Image [orentation]. The endothelial cell nuclei of the sinuses are characteristically plump and closely packed together. Note that the endothelial nuclei bulge toward the lumen of the sinuses - this may help you discern the cords from the sinuses.
Slide 140 thymus neonatal thymus H&E View Virtual Slide
Slide 141 Thymus involuted H&E View Virtual Slide
With low power, look at slide 140 and distinguish between the cortex and the medulla Image. Why is the thymic medulla lighter than the cortex?
Answer
With their dark staining nuclei and little cytoplasm, the abundant T lymphocytes in the cortex give the thymus a dark color. The thymic medulla has far fewer lymphocytes in it and so stains much lighter.
Locate Hassall’s corpuscles slide 140 View Image (which are aggregates of epithelial reticular cells) in the medulla. Try to find other epithelial reticular cells slide 140 View Image [orientation] that are scattered throughout the cortex and medulla the key to identifying them is their large, pale nuclei. Of course, most of the cells with small round nuclei packed into the cortex and medulla are T lymphocytes (when immature, they are called “thymocytes”). Also present are numerous macrophages slide 140 View Image [orientation] which will appear eosinophilic with a foamy cytoplasm or they may even contain engulfed lymphocytes. What are the differences among the various reticular cells and fibers of the lymphoid organs?
Answer
Lymph nodes are filled with reticular cells and fibers. The fibers, made by reticular cells (which are related to fibroblasts) and composed of type III collagen, form a supportive meshwork for lymphocytes and other cells in the cortex and medulla. Reticular cells in the lymph node wrap around the reticular fibers (they are extracellular fibers). This same reticular fiber support is found in the spleen and tonsil as well as the bone marrow. The thymus has epithelial reticular cells. Like reticular cells elsewhere, thymic epithelial reticular cells provide support in the cortex and medulla. Unlike reticular cells, epithelial reticular cells have keratin filaments and are joined by desmosomes. Epithelial reticular cells (which, unlike reticular cells, are true epithelial cells) help make the blood-thymus barrier in the thymic cortex and provide a microenvironment in the thymus for T cells to develop. They also play a crucial role in positive and negative selection of T-cells.
How do lymphocytes leave the thymus?
Answer
To leave the thymus, lymphocytes must survive negative selection to enter the thymic medulla. From the medulla, they intravasate by crossing the walls of venules located at the cortico-medullary junction. Alternatively, they may leave the thymus via efferent lymphatic vessels. There are generally no afferent lymphatic vessels in the thymic cortex because this might allow free antigens to enter the cortex thereby impinging on the positive selection process.
Look at slide 141 and observe the histology of thymic involution, which is basically a replacement of lymphatic tissue by fat. The Hassall's corpuscles slide 141 View Image here are also quite large and a bit bizarre looking. The production of T cells by the thymus in the human adult is generally greatly reduced, but it can continue to produce T-cells even into adulthood.
294 Lymph Node - Subcapsular Sinus and Cortex View Virtual EM Slide
Find the subcapsular sinus and the reticular cells of the node.
296 Lymph Node - Medullary Cord View Virtual EM Slide
Blood vessels are restricted to the medullary cords. Plasma cells occur abundantly in the cords. Review the function and origin of plasma cells. Note that the free, circulating lymphocytes are either small or medium size. Where are the lymphoblasts?
297 Lymph node - Postcapillary High Endothelial Venule View Virtual EM Slide
Note the unusual height of the lining endothelial cells and the lymphocytes of different sizes in transit from the vessel into the lymph node. A small fraction of lymphocytes enter the node through afferent lymphatic vessels.
298 Lymph Node - Detail of medullary lymphatic sinus Medullary Sinus (Lymph Node) View Virtual EM Slide
Observe the loose arrangement of lymphoid tissue in the medulla of lymph nodes. The sinuses interconnect and their lumen is traversed by reticular cells, some of which can trap antigens and some of which are true phagocytes. In addition, reticular cells wrap around the bundles of reticular fibrils and thereby isolate them from lymphocyte access.
303 Spleen White and Red Pulp (Spleen) View Virtual EM Slide
Note the very dense arrangement of lymphoid cells in the white pulp and the loose arrangement of reticular cells, some lymphoid cells and extravasated erythrocytes in the pulp cords between the venous sinuses. Note also the marginal zone and recall that this is where most antigen presentation occurs in the spleen.
306 Spleen - Topography of Marginal Zone Marginal Zone (Spleen) View Virtual EM Slide
The marginal zone is a cell rich region at the interphase between white and red pulp. As it is the region of antigen presentation, a large number of macrophages and different types of lymphocytes reside here.
310 Spleen Red Pulp with Venous Sinus (Spleen) View Virtual EM Slide
Find the venous sinuses and observe the movement of erythrocytes across the wall. The presence of many macrophages in the interstitial space of the red pulp is obvious. What are the functions of the red pulp?
318 Thymus Thymus (Cortex and Medulla) View Virtual EM Slide
Note that the thymus does not have lymph nodules. However, small lymphocytes (thymocytes) are aggregated in the cortex and larger, epithelial reticular cells can be identified in the center (medulla), giving the appearance of a “nodular” area.
319 Thymus - Medulla View Virtual EM Slide
Remember that Hassall’s corpuscles (or bodies) are found only in the thymus.
321 Blood-Thymus Barrier View Virtual EM Slide
Review the components of the blood-thymus barrier.
Click on a question to reveal the answer
What are the functions of the red pulp?
The spleen has two main functions in the body. First, it is a lymphoid organ, providing a place for T cell help and B cell differentiation. This occurs in the white pulp of the spleen. The spleen also serves as a filter of the blood. Arterioles flowing into the cords of the red pulp end and the blood spills into the cords (when blood is not contained in a vessel, it is termed "open circulation"). In order for this blood to re-enter the venous system of the spleen, it must pass from the cords of the red pulp into the sinuses. The walls of the splenic sinuses are made of elongated endothelial cells with transverse running reticular fibers, giving them the look of sheaves on a barrel. These are called "rod cells". Blood cells must wiggle through this "filter" to continue circulating. Those that can't pass through are removed by the macrophages of the spleen.
Where are lymphoblasts found?
Lymphoblasts (sometimes called "large lymphocytes") are typically found in the germinal centers of secondary follicles (which, in turn, may be found in mucosa-associated lymphoid tissue --aka MALT, the cortex of lymph nodes, and the white pulp of the spleen). The presence of lymphoblasts gives germinal centers their lighter appearance, both because of their large size and because of their lightly staining, euchromatic nuclei. Recall that heterochromatic or dense, deeply staining nuclei are characteristic of cells with very limited nuclear transcription; whereas euchromatic or lightly staining nuclei indicate the presence of much transcriptionally active chromatin. Thus, lymphoblasts have euchromatic nuclei because they are transcribing many genes as they differentiate into plasma cells and memory B cells.
Where are macrophages found in the spleen?
You shouldn't see macrophages in splenic sinuses, only in the cords. As cells (especially RBCs) age, they lose their agility. This increased stiffness makes it harder for them to wiggle through the small gaps between the endothelial cells of the splenic sinus. Macrophages often occupy these spaces (within the cords) to "clean up" any cells that don't make it through or that are moving very slowly.
What are some of the defining characteristics of each of the lymphoid organs?
The lymph node is composed of follicles surrounding medullary cords and sinuses. A feature that is characteristic of the lymph node is the post capillary, high endothelial venule. You can occasionally see lymphocytes migrating from the blood into the lymph node if you examine the walls of these vessels. In the palatine tonsil you can see large follicles and a stratified squamous epithelium. One feature of the lymphoid tissue of the tonsil and MALT in general is that its follicles have a "starry sky" appearance. This comes from the numerous, light staining macrophages present, along with lymphocytes and plasma cells, in the germinal centers of the tonsil. The spleen consists of areas of red and white pulp. The spleen can be identified by looking for deep staining areas of white pulp surrounding central arteries. These areas are known as the periarterial lymphatic sheath (PALS for short). Germinal centers of the spleen often run along the PALS. The thymus is unique in that it is the only lymphoid organ with no germinal centers. Germinal centers are made up of B cells that are proliferating and preparing to become plasma cells. You should never see B cells in the thymus. It is a place for the maturation of T cells, which then leave the thymus and enter other lymph tissues. The thymus is composed of lobules. One easily recognizable feature of the thymic medulla is the presence of Hassall's corpuscles. The function of these corpuscles is uncertain, although they do secrete IL-4 and IL-7 and therefore certainly influence the development of the thymus and T-cell maturation.
What are the major antigen presenting cells of the tonsil, spleen and lymph node?
Macrophages are the major APCs in the tonsil and the spleen (although the spleen also has dendritic cells that do this to some extent as well). In the lymph node, dendritic cells are the major antigen presenters, although macrophages in the medullary sinuses also do this to some extent as well.
What is the distribution of B cells and T cells in the lymphatic tissue?
The thymus is entirely composed of T cells, epithelial reticular cells and some macrophages. Occasionally another type of cell will get into the thymus, but it does not belong there. The thymus consists of a cortex and medulla with no germinal centers. Immature T cells are found at the edges of the cortex. As they mature, they migrate deeper into the cortex and eventually leave as mature naïve T cells through the venules of the medulla. In the lymph node, the cortex is made of primary follicles of resting B cells and secondary follicles with germinal centers. The germinal centers are where B cells are undergoing clonal expansion, after binding antigen and receiving T cell help. Most T cells are located deeper in the cortex. Antigen-stimulated helper T cells are formed when antigen is presented to them by dendritic cells (and possibly macrophages), deep in the cortex. B cells also bind their antigen in this region. B cells entering the lymph node travel through the cortex to a follicle. If they have bound antigen in the cortex, they attract antigen-stimulated T helper cells to the follicle, where T cell help occurs. T cell help in the spleen occurs in the PALS. Close to, if not touching, the PALS are follicles of resting B cells, a clone of which may give rise to a germinal center upon proper stimulation.
What is a fiber associated reticular cell?
These are the stellate shaped fibroblasts found in the lymph node that are involved in making reticular (type III collagen) fibers. They are NOT the same as the epithelial reticular cells found in the thymus: epithelial reticular cells s are true epithelial cells derived from the endodermal lining of the third pharyngeal pouch in the embryo (the third pouch is what gives rise to the thymus) whereas reticular cells, like most connective tissue fibroblasts, are derived primarily from mesoderm.
Where do the plasma cells in the lymph node go?
Nowhere. Once a plasma cell differentiates in the lymph node, it generally migrates to a medullary cord in the medulla of the lymph node and begins secreting antibodies that travel throughout the body (first through efferent lymphatics that then drain into venous blood). Once in the medullary cord, the plasma cell generally stays puts. It is worth noting that plasma cells are rarely observed in peripheral blood. The numerous plasma cells found in various tissues in the body traveled in the circulation as naive B lymphocytes until they were stimulated to enter the peripheral tissue and differentiate into a plasma cell locally.
How do cells travel from the blood to the lymph node?
There are many adhesion molecules and receptors expressed both by the high endothelial post capillary venules of the lymph node and on the B and T lymphocytes that allow them to enter the lymph node. This process is called "lymphocyte homing". When appropriate signals are received, cells begin to cross the endothelial cells of the venules. Finally they reach the deep cortex where they can receive T cell help and continue on to the follicles.
Why is the thymic medulla lighter than the cortex?
With their dark staining nuclei and little cytoplasm, the abundant T lymphocytes in the cortex give the thymus a dark color. The thymic medulla has far fewer lymphocytes in it and so stains much lighter.
What are the differences among the various reticular cells and fibers of the lymphoid organs?
Lymph nodes are filled with reticular cells and fibers. The fibers, made by reticular cells (which are related to fibroblasts) and composed of type III collagen, form a supportive meshwork for lymphocytes and other cells in the cortex and medulla. Reticular cells in the lymph node wrap around the reticular fibers (they are extracellular fibers). This same reticular fiber support is found in the spleen and tonsil as well as the bone marrow. The thymus has epithelial reticular cells. Like reticular cells elsewhere, thymic epithelial reticular cells provide support in the cortex and medulla. Unlike reticular cells, epithelial reticular cells have keratin filaments and are joined by desmosomes. Epithelial reticular cells (which, unlike reticular cells, are true epithelial cells) help make the blood-thymus barrier in the thymic cortex and provide a microenvironment in the thymus for T cells to develop. They also play a crucial role in positive and negative selection of T-cells.
How do lymphocytes leave the thymus?
To leave the thymus, lymphocytes must survive negative selection to enter the thymic medulla. From the medulla, they intravasate by crossing the walls of venules located at the corticomedullary junction. Alternatively, they may leave the thymus via efferent lymphatic vessels. There are generally no afferent lymphatic vessels in the thymic cortex because this might allow free antigens to enter the cortex thereby impinging on the positive selection process.
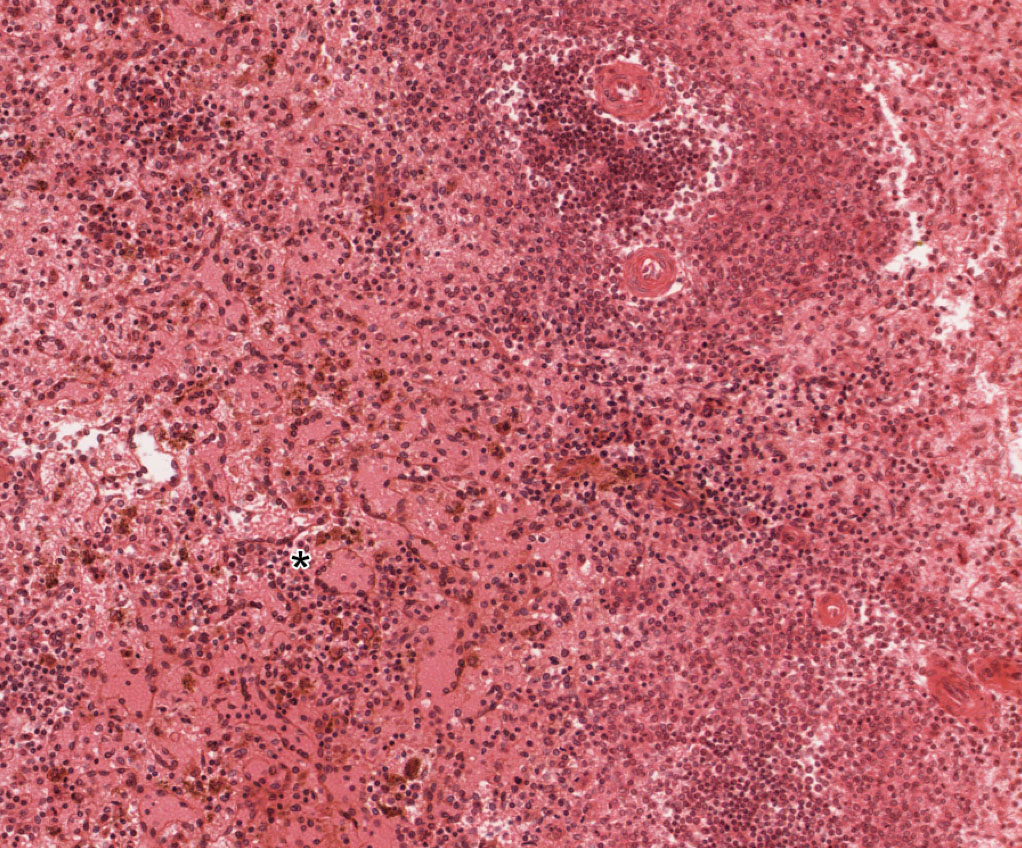
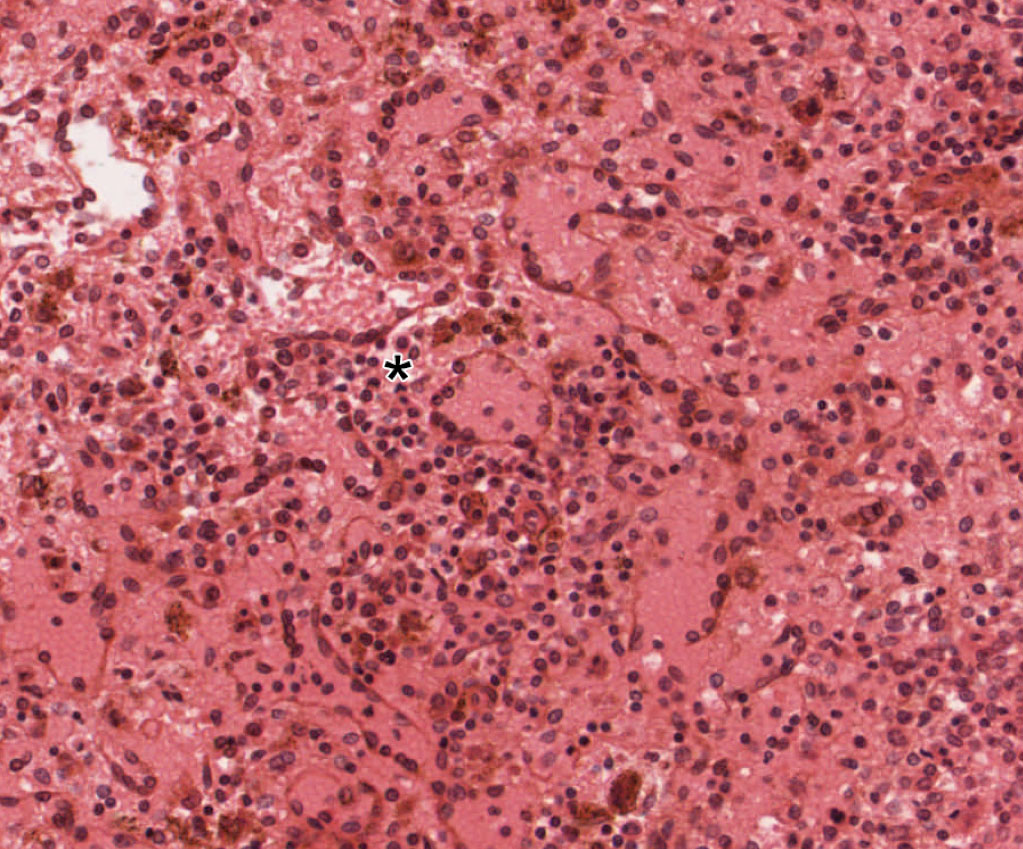
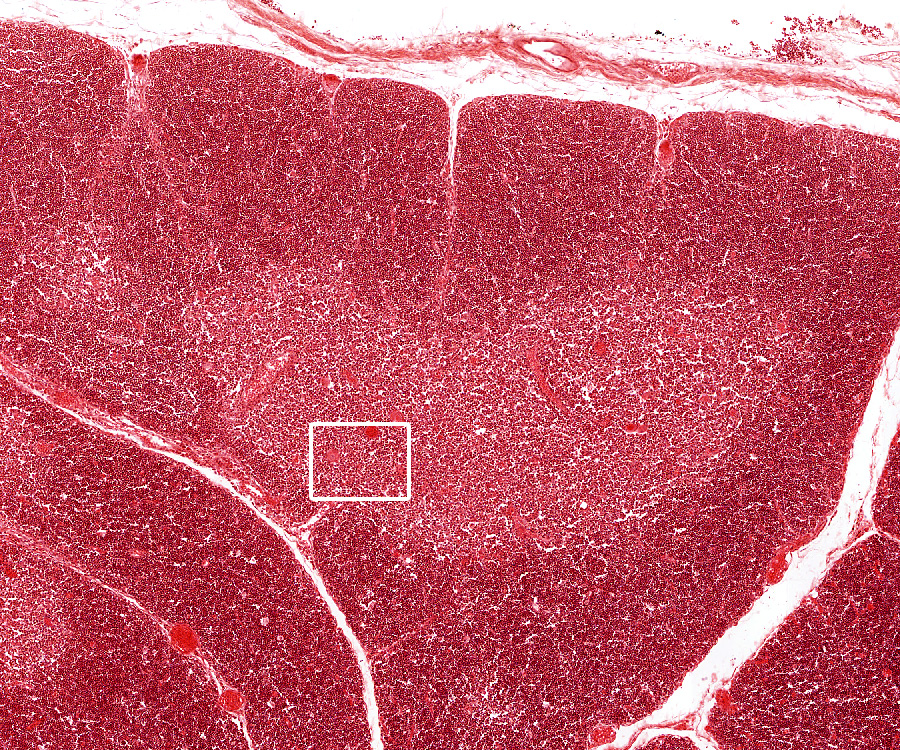
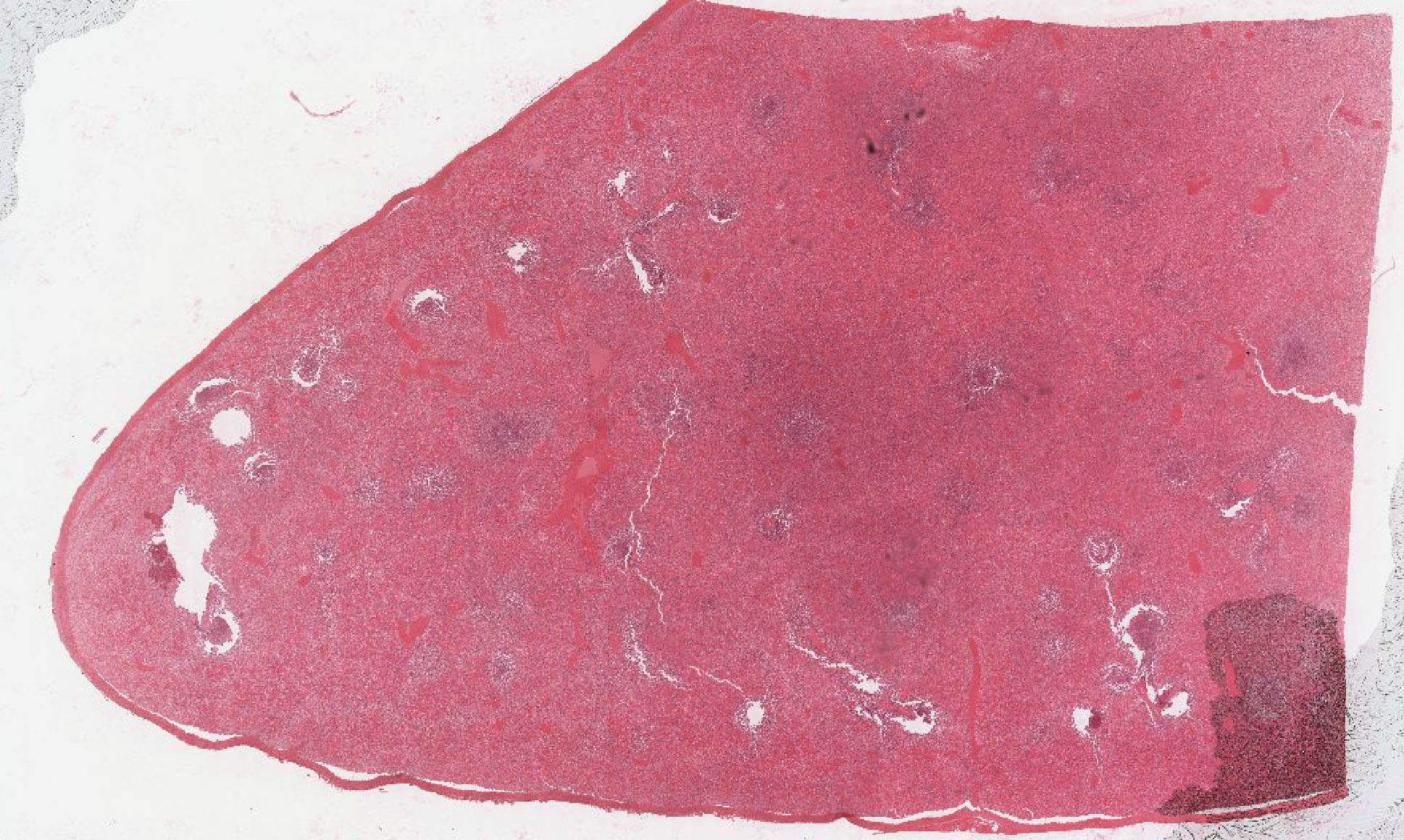
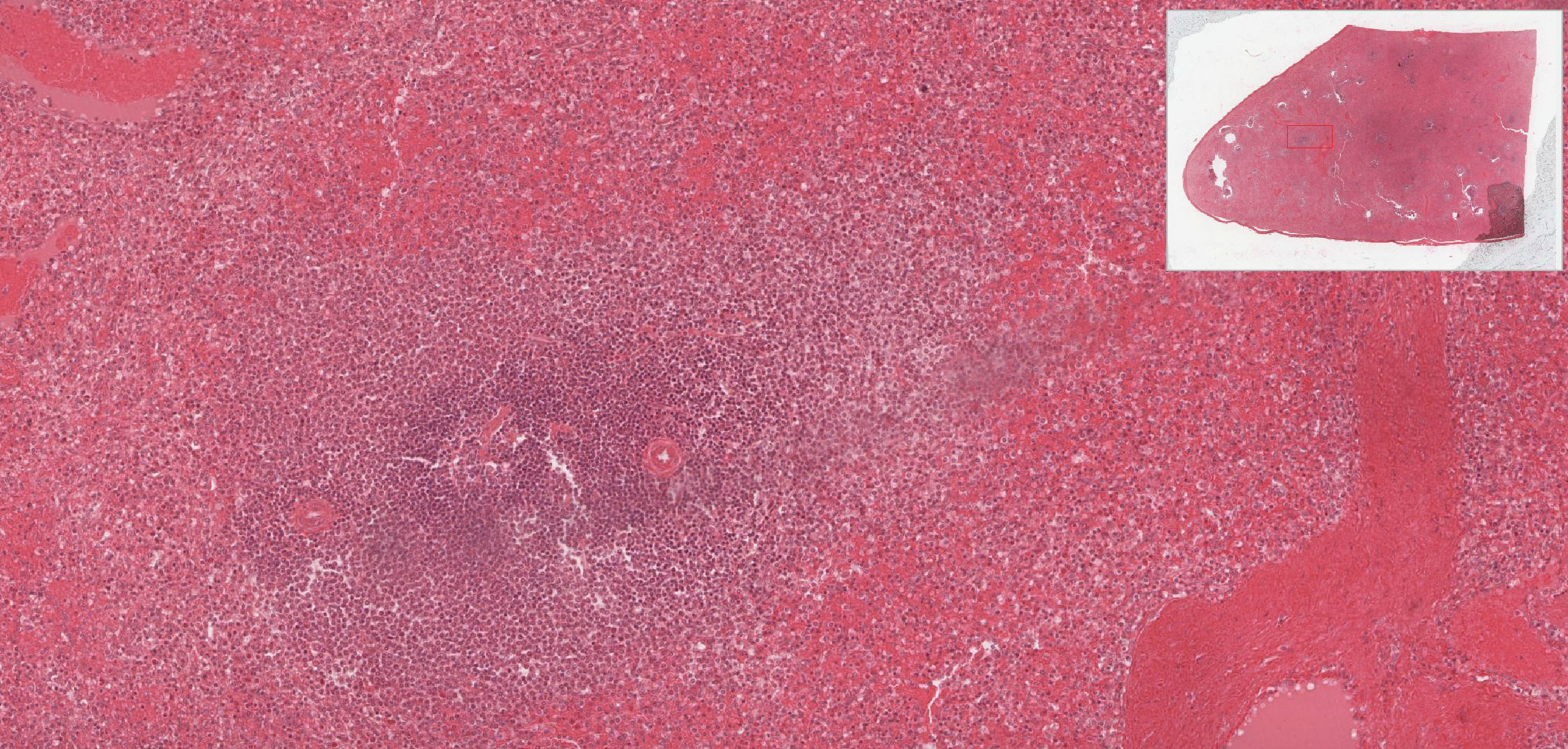
1. Identify the organ depicted by these images.
View Low Mag Image
View High Mag Image
- Spleen
- Tonsil
- Thymus
- Lymph node
- Gut-associated lymphoid tissue
Answer
Correct answer 1. The images show the features of a spleen.
2. Identify the location of the black asterisk.
- A splenic sinus
- A splenic cord
- A lymph node medullary sinus
- A lymph node medullary cord
- The thymic cortex
- The thymic medulla
Answer
Correct answer 1. The asterisk marks a splenic cord. Note the presence of hemosiderin-laden macrophages which can help identify the cords, also note that you can see the outlines of the sinuses with the nuclei of lining cells (rod cells) jutting INTO the lumen of each sinus.
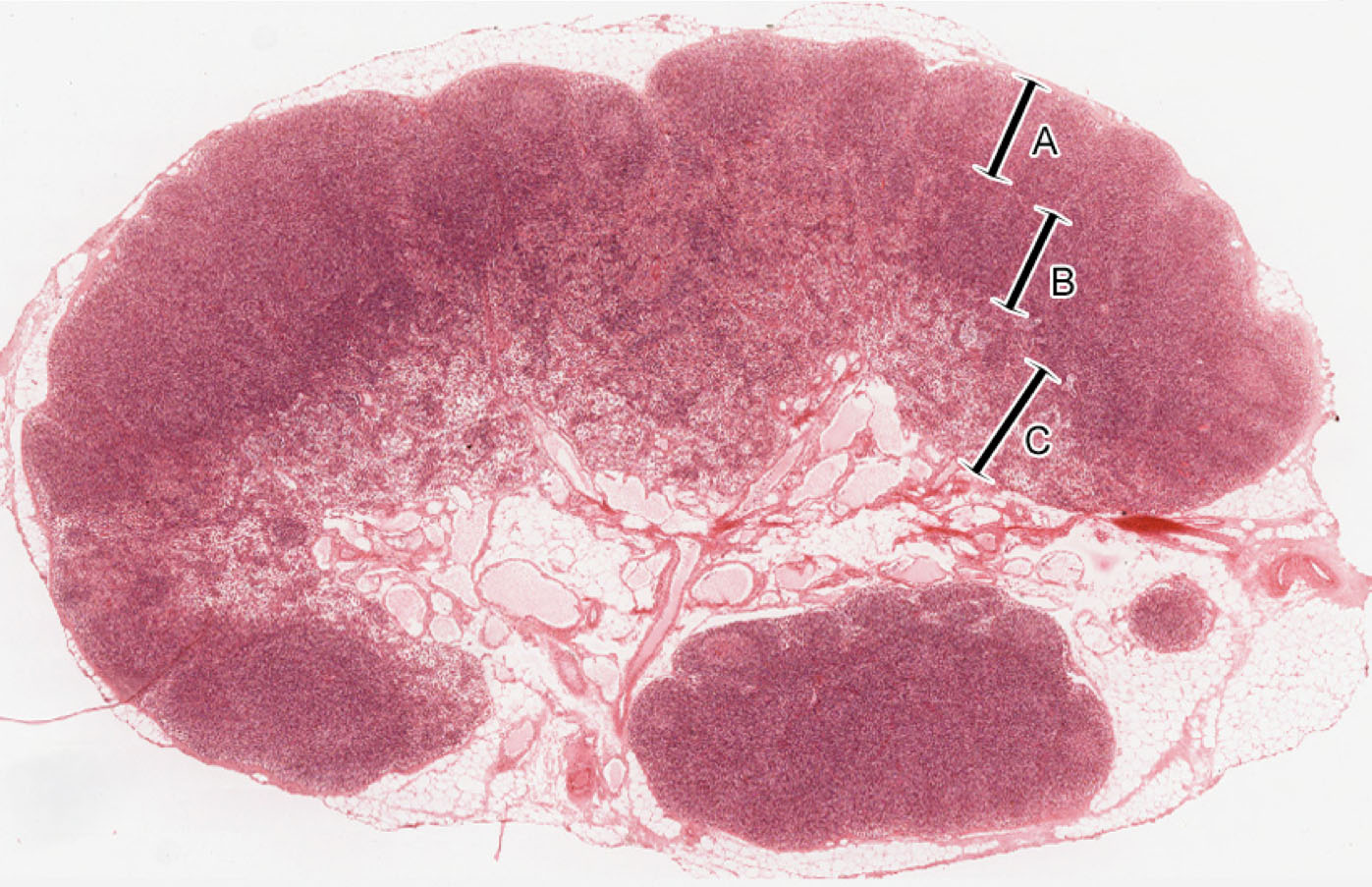
3. In an individual with thymic aplasia (failure of the thymus to develop), which region of a lymph node shown would you expect to be attenuated?
- A
- B
- C
- ALL of the above
- NONE of the above
Answer
Correct answer 2. (B). An individual with thymic aplasia would have no T-cells, so the most dramatic change would be in the deep cortex, which is the T-cell rich zone of a lymph node. The outer cortex would still contain primary follicles since they are B-cell rich, although there wouldn't be many secondary follicles with germinal centers due to a lack of T-cell help. The medulla wouldn't change much. Of course, the prognosis for this individual would not be good as he/she would be highly susceptible to infections.
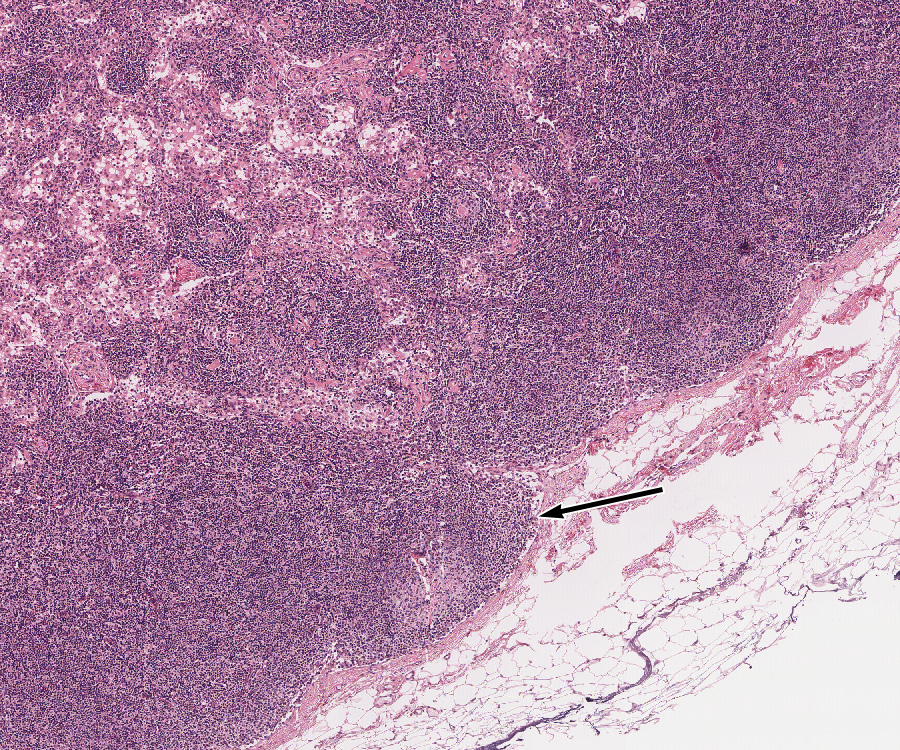
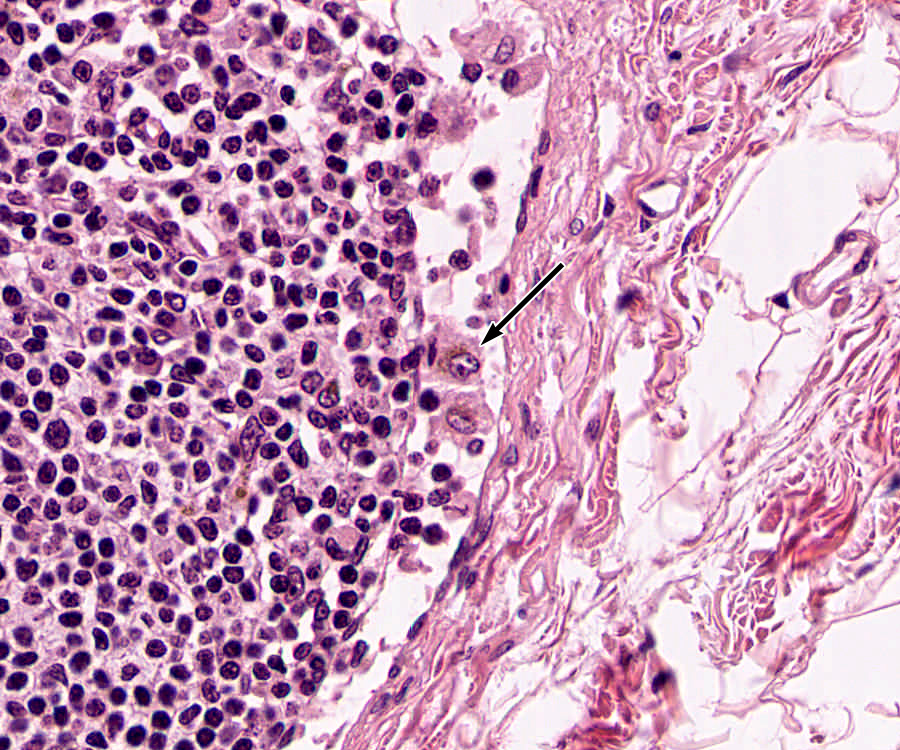
4. Identify the cell indicated by the black arrow.
- An endothelial cell of a high endothelial venule
- A rod cell of a splenic sinus
- An epithelial reticular cell
- A macrophage
- A reticular cell
- A dendritic cell
- A plasma cell
- A T-lymphocyte
Answer
Correct answer 4. A macrophage in the subcapsular sinus of a lymph node. Note the large size, eccentric nucleus, and cell inclusions.
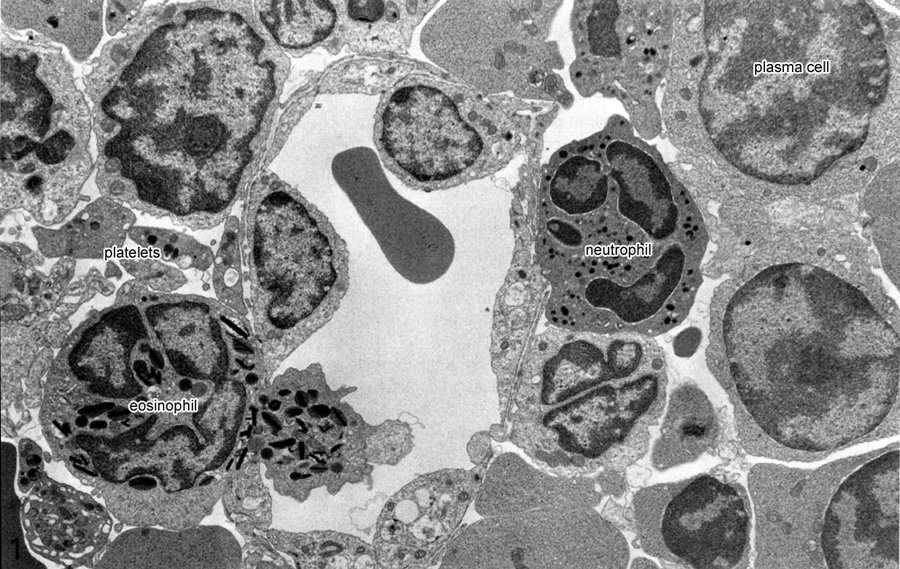
5. The electron micrograph shows an eosinophil traversing a vessel wall. What is the most likely process happening?
- It is entering the deep cortex of a lymph node via a high endothelial venule.
- It is re-entering the bloodstream in a lymph node medullary sinus.
- It is entering the thymic medulla via an afferent lymph vessel.
- It is exiting the thymic medulla via intravasation into a medullary venule.
- It is entering splenic white pulp via an afferent lymph vessel.
- It is re-entering the bloodstream in a splenic sinus.
Answer
Correct answer 6. The presence of blood elements (e.g. platelets) OUTSIDE the vessel should identify this tissue as spleen, leaving only choices 5. and 6.. 5. is incorrect because there generally are no afferent lymph vessels in the spleen. 1. is incorrect because the endothelium is not 'high' - also leukocyte homing in a lymph node is usually restricted T and B-cells and monocytes. 2. is incorrect because medullary sinuses are LYMPHATIC sinuses, not blood sinuses. 3. is incorrect because there are no afferent lymph vessels in the thymus. 4. is possible, but highly unlikely. Mature T-lymphocytes may enter circulation via INTRAVASATION into venules in the thymus. Eosinophils and other granulocytes generally only LEAVE the circulation; they don't re-enter (except in the spleen where all blood cells leave the bloodstream and have to re-enter via the sinuses).
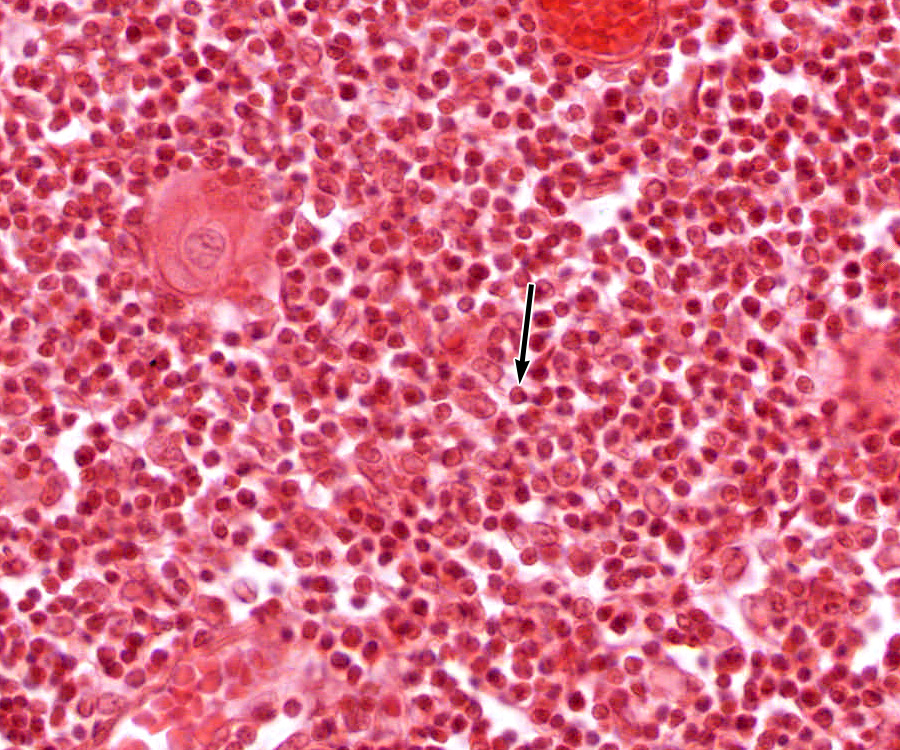
6. Identify the cell marked by the black arrow.
- An endothelial cell of a high endothelial venule
- A rod cell of a splenic sinus
- An epithelial reticular cell
- A macrophage
- A reticular cell
- A dendritic cell
- A plasma cell
- A T-lymphocyte
Answer
Correct answer 8. A T-lymphocyte. First, recognize that these images are from a thymus. The lighter area represents thymic medulla, not a germinal follicle. The morphology of the cell in question is such that it could only be a lymphocyte - although generally one cannot tell B and T-cells apart in routine H&E sections, you should be able to recognize this tissue as THYMUS where there generally are very few B-cells (the functional significance of these B-cells in the thymus is currently unknown).